Table of Contents
What is Vasa Previa?
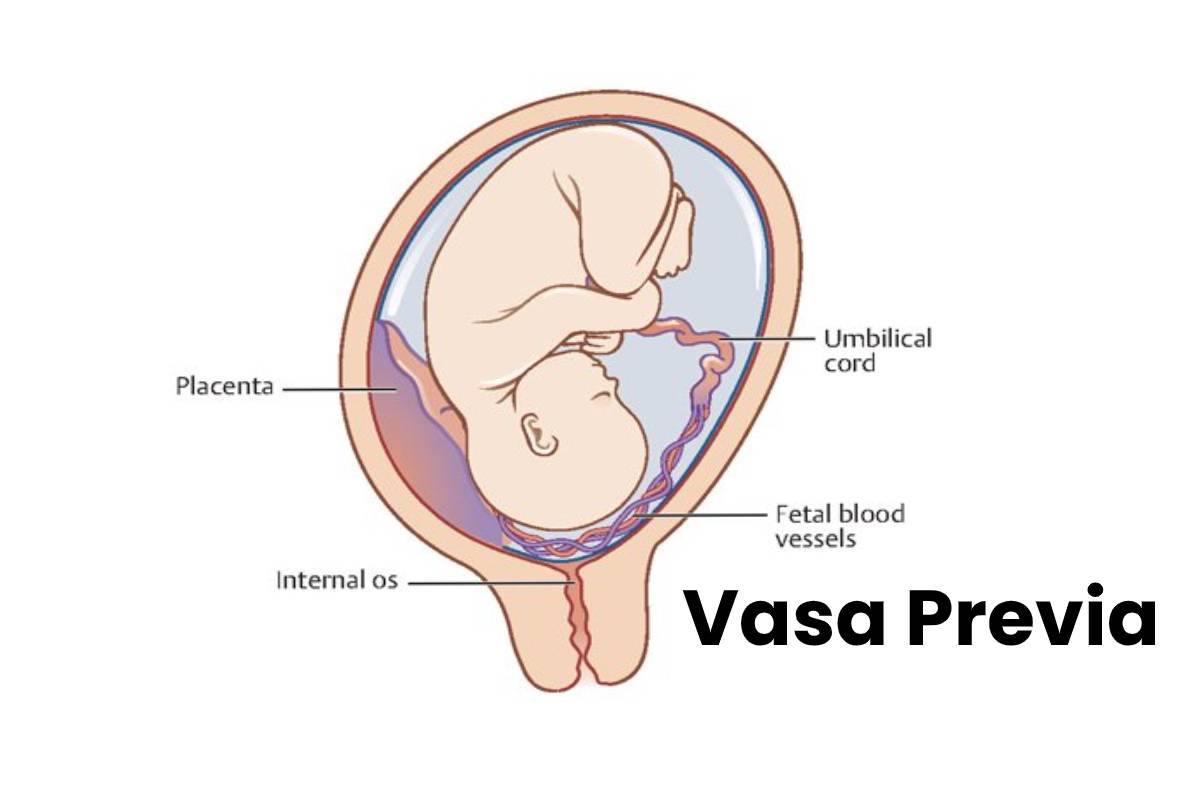
Vasa Previa may present on its own (see figure Vasa Previa ) or placental abnormalities, such as a veiled cord insertion.
In the vellum cord insertion, the umbilical cord vessels pass through part of the amniotic membrane rather than directly into the placenta.
Therefore, the blood vessels are not protected by Wharton’s jelly within the cord, making fetal hemorrhage more likely when the rupture of the fetal membranes.
The prevalence is approximately 1 / 2,500 to 5,000 deliveries. The fetal mortality rate can approach 60% if it does not diagnose before birth.
What are the Symptoms of Vasa Previa?
In a lot of cases, there are no symptoms of vasa Previa at all.
- It frequently goes undetected until labor, when the fetus already distresses or following a stillbirth.
- Pregnant women should seek immediate medical attention if they have any painless vaginal bleeding.
- A sign that a woman might have is if the blood is very dark, a burgundy red.
- The blood of a fetus is naturally lower in oxygen than that of the mother.
- So if the blood is darker than what is typical, it could indicate that it has come from the fetus and not the mother.
Causes and Risk Factors of Vasa Previa
It causes an umbilical cord abnormality called velamentous cord insertion. The umbilical cord moves into the membranes, resulting in unprotected vessels leading to the placenta.
Another cause is the bilobed placenta, where the placenta is in two pieces. In these cases, the vessels may unprotect where they cross in the middle of the two lobes.
You’re at greater risk of vasa Previa if:
- Your placenta is low-lying (placenta previa);
- Your previous birth(s) were by cesarean delivery;
- Pregnancy occurred through in vitro fertilization (IVF);
- You’re pregnant with multiple babies;
- You’ve had prior uterine surgery.
How is it Diagnosis?

- Transvaginal ultrasound
- The Diagnosis of Vasa Previa is suspected by the presentation or by the results of routine prenatal ultrasound.
- At the exhibition, the fetal heart rate pattern, commonly sinusoidal, is usually non-reactive.
- The Diagnosis typically confirms by transvaginal ultrasound. The fetal vessels within the membranes can see passing directly over or near the internal cervical os. Color Doppler flow mapping can use as an adjunct.
- The vasa Previa must distinguish from the funicular presentation (prolapse of the umbilical cord between the presenting part and the internal cervical os).
- The fetal blood vessels can see it wrapped in Wharton’s jelly covering the cervix.
- In the cord presentation, the umbilical cord moves away from the cervix during ultrasound evaluation; in this, the line fix in place.
Treatment of Vasa Previa

- Prenatal monitoring to detect cord compression
- Cesarean section
Prenatal management of it is controversial, in part because randomized clinical trials are insufficient.
In most centers, stress-free tests perform twice a week, starting at 28-30 weeks. The motive is to detect compression of the umbilical cord.
Admission is often offered for continuous monitoring or non-stress testing every 6 to 8 hours around 30 to 32 weeks. Corticosteroids use to accelerate the maturity of the fetal lungs.
Emergency cesarean delivery indicates if any of the following occur:
- A premature rupture of membranes occurs.
- Vaginal bleeding continues.
- The fetal state is not reassuring
No at all of these problems are present, and labor does not occur, doctors may offer to schedule a cesarean delivery.
Cesarean delivery between 34 and 37 weeks has suggested, but the exact timing is controversial; some tests favor delivery at 34 or 35 weeks.
Key Concepts
- Vasa Previa can accompany other placental abnormalities, such as vellum insertion, which increases the risk of fatal bleeding when the fetal membranes rupture.
- It bases on symptoms and findings during a routine prenatal ultrasound.
- Use transvaginal ultrasound to confirm vasa Previa and distinguish it (fixed umbilical cord) from the presenting cord (mobile cord).
- Seek stress-free testing cord compression, possibly twice weekly beginning at 28-30 weeks.
- Perform a planned cesarean section, or if there is premature rupture of the membranes. It continuous vaginal bleeding or the fetal state is non-reactive, perform an emergency cesarean delivery.
Conclusion
Vasa Previa doesn’t cause any physical health risks to the mother, but the baby’s troubles can be significant and ultimately lose their lives.
More than half of the cases of vasa Previa n’t detect in pregnancy result in stillbirth.
However, if the condition diagnoses in pregnancy, then the baby’s chances of survival are excellent.
It’s essential to remember that while this condition causes concern, it’s also very uncommon. And also the most extensive studies report that it only finds in up to 4 of 10,000 pregnancies.